Table of Contents
If you have been told that you are not suitable for standard implant treatment because of severe bone loss in your upper jaw, you are not alone. Many patients come to this point after years of missing teeth, failed implants, or being advised that there is not enough bone to support regular solutions. At this stage, people are often confused, disappointed, and unsure whether there is still a reliable option for fixed teeth. Zygomatic dental implants were developed exactly for these situations, offering a different approach when traditional methods are no longer possible. This guide focuses on the real questions patients ask before choosing this treatment, helping you understand how it works, who it is for, and what you can realistically expect from the process.
Why was I told that regular implants are not suitable for me?
This is one of the most frustrating things patients hear during a consultation. Many people arrive expecting a straightforward solution, only to be told that regular implants may not work for them. The reason is usually related to bone loss in the upper jawbone, which often develops gradually after tooth loss. When teeth are missing for a long time, the bone that once supported them begins to shrink, reducing both volume and bone density.
Traditional implant systems rely on sufficient bone in the upper jaw to stay stable over time. If this area no longer has enough quality or thickness, placing standard implants becomes risky. In such cases, implants may fail to integrate properly, loosen over time, or never achieve the stability required for long-term success. This is not a reflection of the patient’s overall health, but rather a limitation of the available bone structure.
For many patients, this news comes after previous treatments or even failed implant attempts. Hearing that conventional solutions are no longer possible can feel discouraging. However, it is important to understand that this does not mean fixed teeth are out of reach. It simply means that a different treatment option may be needed one that does not depend solely on the weakened bone of the upper jaw.
What exactly are zygomatic implants and how are they different?
After being told that standard solutions may not work, patients usually ask this question next. The term zygomatic implants can sound unfamiliar and even intimidating at first, especially if it has never been mentioned before. In simple terms, this approach was designed for people who do not have enough bone in the upper jaw to support conventional solutions.
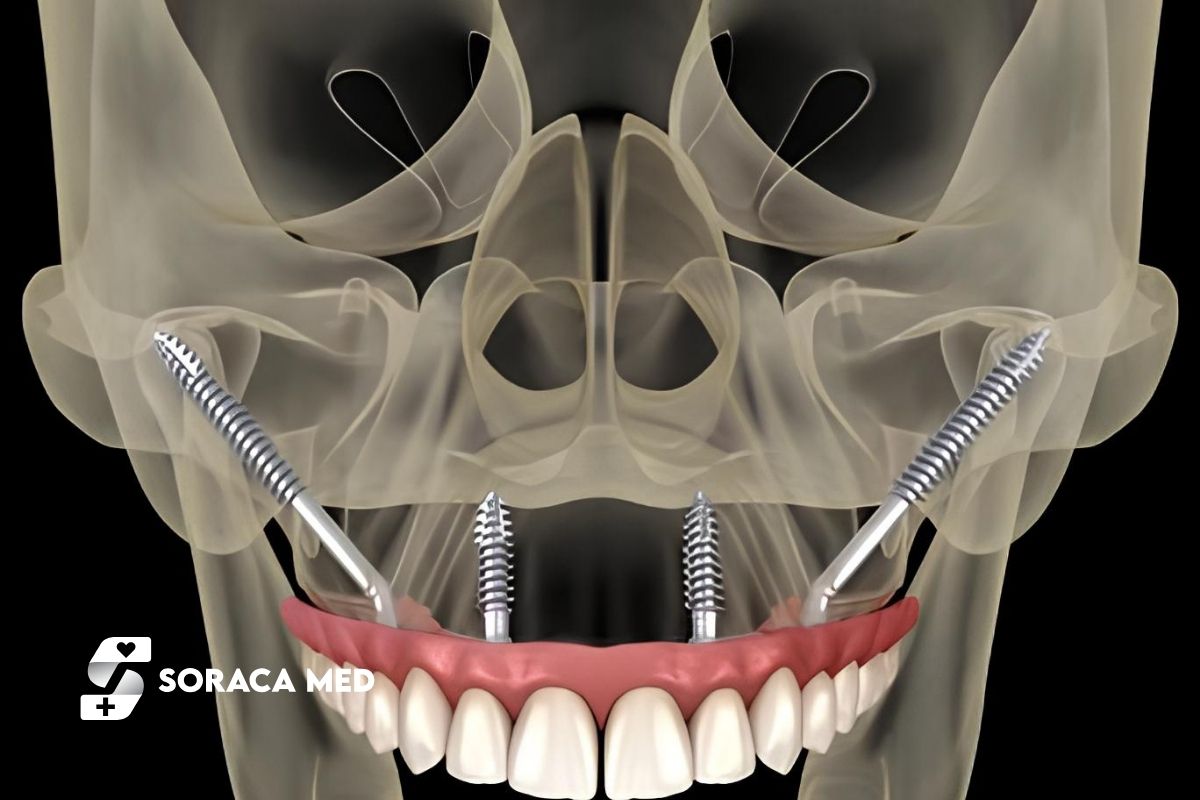
Unlike regular systems that rely on the weakened upper jawbone, these implants are placed in a stronger area of the face. They are longer and are positioned so that the implants are anchored in a denser structure, providing reliable support even when significant bone loss is present. This is why zygomatic dental solutions are often recommended when other methods have already failed or are considered too risky.
For patients, the main difference is not only where the implant is placed, but how stability is achieved. Instead of depending on bone volume that may no longer exist, this method uses natural anatomical strength to secure the implants. As a result, many people who were previously told they had no fixed-tooth options discover that a predictable solution is still possible.
Understanding this difference often brings relief. It shifts the focus away from what cannot be done toward what can be achieved with the right approach and an experienced surgical team.

Do zygomatic implants anchor in the cheekbone?
This question is often asked with hesitation, and that reaction is completely understandable. Hearing that an implant may anchor in the cheekbone can sound alarming at first, especially for patients who are already anxious after being told they have limited options. What matters most here is understanding why this area is chosen and how it actually improves safety.
The cheekbone is one of the strongest and most stable bones in the facial structure. Unlike the upper jaw, it is far less affected by tooth loss and does not shrink in the same way over time. By placing the implants in this area, surgeons can achieve additional stability that is simply not possible in severely weakened jawbone. This strong anchorage is what allows fixed teeth to be supported even when the upper jaw can no longer provide reliable support.
For patients, this does not mean a change in facial appearance or function. The implant remains completely internal and is not visible from the outside. Its purpose is purely structural to create a secure foundation for a fixed set of teeth when other methods are no longer dependable. Understanding this often helps patients move past the initial fear and focus instead on the long-term benefit: stability, comfort, and confidence when eating and speaking.
Am I a candidate if I have severe bone loss in my upper jaw?
This is one of the most personal questions patients ask, often after hearing “there is not enough bone” more than once. Severe bone loss in the upper jaw does not automatically mean that fixed teeth are no longer possible. In fact, this situation is one of the main reasons why alternative solutions were developed in the first place.
Patients who are usually considered for this treatment option include those who have been missing teeth for many years, wear removable dentures, or have experienced failed implant attempts in the past. In these cases, the remaining bone in the upper jaw is often no longer strong or thick enough to support standard approaches. This can feel discouraging, but it does not close the door on treatment.
What matters most is not just how much bone has been lost, but where stable support can still be achieved. A detailed examination and imaging are essential to determine whether this approach is suitable. With the right assessment and a personalized treatment plan, many patients who were previously told they had no solution are surprised to learn that they are still candidates for fixed teeth.
At this stage, the focus shifts from what is missing to what is still possible finding a safe and predictable way to restore comfort, function, and confidence.
Is a bone graft or sinus lift still necessary?
This is often the question that determines whether patients feel hopeful again or remain hesitant. Many people considering implant treatment have already been told that they need extensive procedures such as a bone graft or a sinus lift, sometimes over multiple stages and long healing periods. Understandably, this can feel overwhelming.
In cases of severe bone loss in the upper jaw, traditional approaches rely on rebuilding missing bone before implants can be placed. While this may work for some patients, it is not always predictable and often requires additional surgeries, longer treatment times, and extended recovery. This is where alternative solutions can make a meaningful difference.
Because this approach does not depend on the weakened bone in the upper jaw for support, a bone graft or sinus lift is often not required. By anchoring the implants in a stronger area, the need to rebuild insufficient bone can be reduced or completely avoided. For many patients, this simplifies the process and shortens the overall treatment timeline.
That said, every case is unique. A thorough evaluation is still essential to determine what is truly necessary. The goal is not to add procedures, but to create the safest and most efficient plan possible one that respects both the patient’s comfort and long-term outcome.
How is the implant surgery performed?
For many patients, the idea of implant surgery is more stressful than the condition itself. Questions about pain, anesthesia, and recovery usually come up long before the actual procedure is discussed. Understanding what happens step by step can significantly reduce this anxiety.
The procedure is carefully planned in advance using detailed imaging and measurements. This preparation allows the surgical team to place the implants safely and precisely. On the day of surgery, the treatment is usually performed under general anesthesia or deep sedation, so patients do not feel pain or discomfort during the procedure. The goal is to make the experience as comfortable as possible.
Because zygomatic implant treatments are designed for cases with advanced bone loss, the surgical approach is different from standard methods. The implants are positioned to achieve immediate stability without relying on weak upper jaw bone. In many cases, this stability allows patients to move forward more quickly in the treatment process compared to traditional techniques.
After the procedure, some swelling and mild discomfort are normal, especially in the first few days. However, most patients are surprised to find that recovery is manageable with proper aftercare and guidance. Clear instructions, medication, and follow-up support play a key role in helping patients feel secure throughout the healing phase.
Will I leave with replacement teeth or temporary teeth?
This is often the turning point in a patient’s decision-making process. Many people considering this treatment are not only concerned about surgery itself, but also about how they will look and function immediately afterward. The idea of leaving without teeth, even temporarily, can be a major source of anxiety.
In many cases, patients can leave the clinic with replacement teeth shortly after the procedure. These are usually temporary but fixed teeth, designed to restore basic function and appearance while healing takes place. Although they are not the final prosthetic solution, they allow patients to speak, smile, and eat soft foods with confidence during the recovery period.
The final set of teeth is placed only after proper healing and stabilization have occurred. This step-by-step approach helps ensure long-term success and durability. It is important to understand that temporary teeth are not meant to be perfect in shape or strength, but they play a crucial role in maintaining comfort and quality of life while the treatment progresses.
Clear communication at this stage is essential. Knowing what to expect and when helps patients feel prepared rather than surprised, making the overall experience far more reassuring.
Is recovery more difficult compared to traditional dental implants?
This question usually comes from patients who have either had implant treatment before or know someone who has. It is natural to assume that a more advanced procedure must mean a harder recovery. In reality, the experience is often different from what patients expect.
Compared to traditional dental implants, the recovery process may feel similar in the first days, with swelling and mild discomfort being the most common effects. However, because this approach avoids multiple additional procedures in many cases, some patients actually find the overall healing process more straightforward than treatments involving staged surgeries and long waiting periods.
What makes the difference is not just the technique, but how the treatment is planned and executed. Proper pain management, clear post-operative instructions, and close follow-up all play a major role in how patients feel during recovery. Most people are able to return to light daily activities relatively quickly, focusing mainly on rest and soft foods during the early phase.
It is important to remember that every patient heals differently. Comparing recovery timelines can be misleading. What matters most is achieving a stable, long-term result with the least amount of stress and interruption to daily life.
How long do zygomatic implants last?
This question usually reflects a deeper concern: patients want to be sure that the effort, time, and emotional investment they are making will truly pay off. After dealing with missing teeth or failed treatments, durability becomes just as important as aesthetics.
Because these implants are placed in a strong and stable bone structure, where implants are anchored with greater support, they can offer long-term reliability when planned and performed correctly. The additional stability provided by this anchorage plays a key role in maintaining function over the years, especially in patients who previously lacked sufficient support in the upper jaw.
That said, longevity is never based on the implant alone. A well-designed treatment plan, precise surgical execution, and proper oral care all contribute to long-term success. Regular follow-ups and good hygiene habits help ensure that the surrounding tissues remain healthy and supportive.
For many patients, understanding this brings reassurance. The goal is not a temporary fix, but a stable solution that supports everyday life eating, speaking, and smiling with confidence for many years to come.
What risks should I realistically know about?
Most patients are not looking for perfection; they are looking for honesty. After hearing about complex treatments, it is natural to wonder what could go wrong and whether the risks are truly manageable. Understanding this clearly helps patients make decisions with confidence rather than fear.
As with any advanced procedure, there are potential risks, especially when the anatomy of the upper jaw is already compromised. These may include swelling, temporary discomfort, or delayed healing. However, the most important factor in minimizing risks is proper planning. A personalized treatment plan, created after detailed evaluation and imaging, allows the surgical team to anticipate challenges and address them before they become problems.
Experience also matters greatly. This type of procedure requires specific surgical expertise and a clear understanding of facial anatomy. When performed by an experienced team, complications are significantly reduced, and outcomes become far more predictable.
What reassures many patients is knowing that risks are not ignored or minimized but managed. Being informed, asking questions, and understanding the process helps turn uncertainty into clarity and trust.
Is this treatment done in one visit or multiple stages?
This question is especially important for patients traveling from abroad or those who need to plan time away from work and daily responsibilities. After hearing about complex dental procedures, many people worry about repeated visits and long treatment timelines.
In many cases, this treatment can be completed in fewer stages compared to conventional approaches. Because the implants achieve strong initial stability, the process often moves forward more efficiently. For suitable patients, the surgical phase and placement of temporary fixed teeth can be done within a single visit, reducing the need for multiple trips.
However, it is important to understand that every case is different. The number of stages depends on individual anatomy, healing response, and the overall treatment plan. Some patients may require additional time to ensure optimal results before final teeth are placed. This step-by-step approach is not a delay, but a safeguard for long-term success.
Clear planning from the beginning helps patients feel in control. Knowing how many visits are required, how long each step takes, and what to expect between stages makes the entire journey far less stressful.
Who should perform zygomatic implant treatments?
This is a question patients often ask after they start understanding how specialized this approach is. Once it becomes clear that this is not a routine procedure, trust and experience naturally come to the forefront. Patients want to know not only if the treatment works, but who should be responsible for performing it.
This type of implant surgery requires advanced surgical training and a deep understanding of facial anatomy. The placement involves working around sensitive areas and achieving precise angulation to ensure long-term stability. Because the upper jawbone is no longer the main source of support, experience in alternative anchoring techniques becomes essential.
Not every clinic or practitioner offers this treatment, and that is not necessarily a negative thing. It simply reflects the level of expertise required. Patients benefit most when the procedure is carried out by a team that regularly performs these treatments and follows a structured, individualized approach rather than a one-size-fits-all method.
Feeling confident in the team behind the treatment often brings as much peace of mind as the solution itself. Knowing that your case is evaluated carefully and handled by experienced hands helps turn a complex decision into a manageable one.
Our Bookimed Reviews
Our Google Reviews
Frequently Asked Questions (FAQ)
Is this treatment painful?
Most patients are surprised by how manageable the experience is. The procedure itself is performed under anesthesia, so pain is not felt during surgery. Afterward, some swelling or discomfort is normal, but it is usually controlled well with prescribed medication and proper aftercare.
How long does the surgery take?
The duration depends on the individual case and the number of implants placed. In general, the surgical phase takes a few hours. Detailed planning beforehand helps ensure that the procedure is efficient and predictable.
Will my face look different after the procedure?
No visible changes occur in facial appearance. The implants are placed internally and are not noticeable from the outside. Their purpose is structural to support fixed teeth without affecting facial expression or shape.
Can both sides of the upper jaw be treated at the same time?
Yes, in many cases both sides can be treated during the same procedure. This approach often reduces overall treatment time and avoids multiple surgeries. The final decision is based on individual anatomy and the personalized treatment plan.
What happens if I have already had failed implants before?
Previous implant failure does not automatically rule out this option. In fact, many patients consider this approach precisely because earlier solutions did not work. A thorough evaluation helps determine whether sufficient stable support can still be achieved.
Is this treatment suitable for older patients?
Age alone is not a limiting factor. What matters more is general health and the condition of the supporting structures. Many older patients successfully undergo treatment and benefit from improved comfort and function.
How soon can I eat normally again?
Patients usually start with soft foods during the early healing phase. As recovery progresses and stability improves, a gradual return to normal eating is possible. Your care team will provide clear guidance at each stage.
What if I am nervous or anxious about surgery?
Feeling anxious is completely normal. Clear communication, proper preparation, and knowing what to expect often reduce fear significantly. Many patients report that the experience is far less intimidating than they initially imagined.
How important is follow-up after treatment?
Follow-up care is essential for long-term success. Regular check-ups help ensure that healing progresses well and that the final teeth function comfortably and predictably over time.

